Chen Ding-shinn vs. Hepatitis B
Chang Chiung-fang / photos Hsueh Chi-kuang / tr. by Chris Nelson
August 2007

Hepatitis is Taiwan's "na- tional disease." Currently, 16% of Taiwan's population carries hepatitis B, the highest rate in the world. Nevertheless, the superb results of Taiwan's hepatitis B prevention efforts have set a historical precedent in the medical and public health fields.
In the 1960s, little was known in Taiwan about this disease, but now Taiwan has become a model for the world, having reduced the number of hepatitis B carriers by 500,000 and halted the curse of mother-to-child infection.
A key figure in this effort, the one who has made the greatest contribution, is Professor Chen Ding-shinn of National Taiwan University's Hepatitis Research Center, an authority on digestive medicine who is set to step down as dean of NTU's College of Medicine in August 2007.
"This is a pomelo tree and that's a Taiwan flamegold," says the 64-year-old Chen as he eagerly introduces the trees on the old college grounds, brimming with pride as if they were his own. Some of the older trees were his companions throughout his journey from lowly student to lofty deanship at the College of Medicine. Chen himself is like an old tree that has taken root here: he's a native born and bred medical scientist. He has been dubbed the Father of Hepatitis, yet despite having undertaken two short-term training sessions abroad, he has no formal degrees from overseas, not even a master's.
With his dogged determination to make the right contributions to Taiwan at the right time, Chen has devoted his mental energies to the prevention of hepatitis B, a national disgrace that has done serious harm in Taiwan. And as a consequence he has gained a worldwide reputation.
Chen's war against hepatitis didn't start by accident. When he was in sixth grade, he had to recuperate at home for a month after a bout with acute hepatitis A. Then when he was a senior at the NTU College of Medicine, his father contracted liver cancer and died a quick and untimely death. Having grappled twice with the specter of disease, the first time in ignorance and the second time at a loss what to do, Chen vowed to research liver disease in order to subdue this dreaded ailment.
Chen chose the path of research after completing his residency. His mentor was Professor Sung Jui-lou, then NTU's authority on liver disease, and thus began Chen's development in the field of liver disease research.
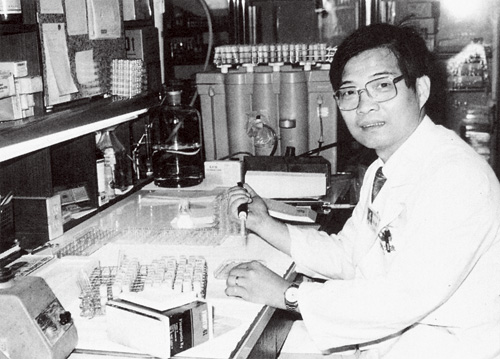
Solutions to clinical problems need to be sought in the lab. Here, Chen plays the dual role of doctor and scientist.
A quiet but precious organ
Perhaps due to genetic reasons, liver disease has been prevalent in Asia for a long time. Liver cancer is the most common cancer in Taiwan, mainland China, Thailand and South Korea. Among the top ten causes of death in Taiwan, two are liver-related: cancer (with liver cancer holding the top spot) and chronic liver disease. This underscores the importance of liver disease research and prevention in Taiwan.
Weighing in at between 1,400 and 1,600 grams, the liver is the largest and heaviest internal organ in the human body, as well as the one with the most diverse functionality. All protein synthesis, carbohydrate and fat metabolism, coagulant production, energy supply to the muscles, and detoxification in the human body depend on it.
Despite the preciousness of this organ, we don't usually notice pain or discomfort when its cells are damaged.
Chen states that when the liver is inflamed due to infection or injury, nine out of ten people don't exhibit symptoms, while the rest experience minor signs like fatigue, loss of appetite, nausea, vomiting, upper abdomen aches, fever or jaundice. The liver has the ability to regenerate, but when it's repeatedly subjected to severe inflammation that exceeds its ability to recover, the resulting abnormal proliferation of connective tissue and excessive deposits leads to the replacement of liver tissue with fibrous scar tissue, gradually diminishing liver function. This is known as cirrhosis.
"Prevention is the best way to protect the liver from damage," says Chen. Viruses, alcohol, certain medicines, chemicals and tainted foods can damage the liver, and the most common among these, and those with the greatest effect, are viruses.
Viral hepatitis can be divided into five types, designated A through E. Of these, types A and E enter the body orally and usually cause acute sickness, while B, C and D are transmitted through blood or other bodily fluids, and are more likely to result in chronic liver disease.
Hepatitis A is contracted through food and drink, and more than 20 years ago, when eating habits and hygiene standards were poor, 99% of adults in Taiwan had hepatitis A antibodies (meaning they had contracted the disease but recovered fully). It can be said that practically everyone had "hit the jackpot."
Hepatitis D cannot cause disease by itself: it depends on co-infection with the hepatitis B virus (HBV). Thus, hepatitis B prevention also happens to prevent hepatitis D. And hepatitis E, with clinical symptoms similar to hepatitis A, is uncommon in Taiwan. It's a self-healing disease with a very low mortality rate, so not much effort has been put into researching it.

This past February, Chen shared his experience in hepatitis prevention at Academic Sinica. In his talk entitled "Fighting Hepatitis," he appealed to citizens not to take the lack of early symptoms lightly.
A reluctant world leader
In the first half of the 20th century, human knowledge of liver pathology was quite limited, and it was only through epidemiological research that it was learned that hepatitis is infectious.
Among the five types of viral hepatitis, hepatitis B is the most damaging to the liver because it develops into chronic liver disease. Research has found that 80% to 90% of cases of chronic liver disease and liver cancer in Taiwan are caused by chronic infection of HBV.
In 1965, the "Australia antigen" (the surface antigen of HBV) was discovered by American physician Baruch S. Blumberg, sparking a wave of research into viral hepatitis. In 1969, Professor Sung Jui-lou of NTU began researching hepatitis B in Taiwan. Then in 1972, Chen started collaborating with Sung in his research.
From complete ignorance about HBV to the gradual discovery of the vectors of infection and methods for prevention, Chen forged ahead unflaggingly in his research, removing layer after layer of hepatitis B's perplexing shroud.
First, after learning how to test for hepatitis B, the research team began carrying out hepatitis B screenings in Taiwan. From small-scale tests they found to their surprise that Taiwan had the world's highest hepatitis B infection rate.
Then to lower testing costs, Sung sent Chen to Japan to study the highly accurate but inexpensive hemagglutination assay method. Chen studied day and night for four months, losing eight kilograms in the process, and after bringing the new technology back to Taiwan the team began extensive screening in order to learn how widespread hepatitis B was.
The test results were shocking: "By around age 20, about 70% of the people had been infected, and by age 40 the infection rate was as high as 90%," says Chen. Compared to the US with 15% and Japan with 30%, Taiwan's infection rate was surprisingly high. More frightening was that as many as 16% of them, a total of about 3 million, would become chronic carriers, over three times the global average of 5%.

There are 3 million hepatitis B carriers in Taiwan, of whom as many as 1.8 million are potential cancer patients. The impact on families and society is grave.
The great hepatitis B riddle
Having identified hepatitis as Taiwan's super-villain, the next step in the conundrum was to discover its infection routes.
Hepatitis B has four subtypes. In his investigations Chen found that among citizens of Taiwan, who originate from all over China, those of northern Chinese origin hosted the North China subtype. Even their children, who were born and raised in Taiwan, carried the same subtype. From this Chen inferred that the main source of infection of hepatitis B in Taiwan is not the greater environment, but the family.
Through infected family members, Chen continued tracing the paths of infection, drawing charts of family infection routes, thereby solving the riddle of transmission. The greatest mode of infection of hepatitis B in Taiwan occurred during birth: so-called "vertical transmission" caused when the baby passes through the birth canal.
But why does hepatitis B cause cirrhosis and liver cancer? So that they could progress from protein research to DNA research, Sung sent Chen abroad a second time to study the burgeoning field of molecular biology. In 1979, after undertaking a year of research at the National Institutes of Health in the US, Chen verified that liver cancer tissue showed signs of insertion of HBV genes. The reason for this still awaits further research.
Now that they knew that cirrhosis, liver cancer and hepatitis B are related, and that the main vectors of infection are known, what could be done for prevention?
Under the advocacy of Chen and his associates, the Executive Yuan approved a hepatitis B prevention program in 1981, and Taiwan's war on hepatitis B began in earnest. With the National Science Council placed in charge of basic research, the Ministry of Education responsible for training researchers and health instructors and the Department of Health spearheading preventive measures, the battle against hepatitis B raged.

When infected by hepatitis, 90% of victims show no symptoms. Blood screening is the best way to identify chronic carriers so early treatment can be administered.
Taiwan's experience
In 1984, Taiwan set a precedent by launching the world's largest hepatitis B vaccination program. Starting with prenatal screening, the program began by focusing on newborn babies of female carriers, and in 1986 it was expanded to all newborns and then to pre-school-aged children, school-aged children and family members of carriers.
For those at the forefront of this program, risk and opposition were inescapable. "Nobody in the world has done it this way before, why should we be the first? Is it because the researcher wants fame or fortune?" "Newborns don't need to be vaccinated in Europe or America, so why should Taiwan's babies be the guinea pigs?" The clamor of questions was relentless, but it didn't shake Chen's confidence. "Seeing patients vomiting blood and swelling with abdominal fluid every day and watching them die painful deaths was truly unbearable," says Chen. At that time, those who carried out hepatitis B prevention were clinical physicians on the front lines directly in contact with patients. "Though some people worried about the side effects of the vaccine, such a theoretical worry is not as serious as the real damage caused to carriers by liver disease," says Chen.

Mother-to-child (or vertical) transmission is the main vector for hepatitis B in Taiwan. Vaccination during infancy is the only way to block this mode of transmission.
Why start with newborns?
"If you're clear about hepatitis B's high prevalence and specific routes of infection, you'll naturally want to cut off the transmission between mother and child," says Chen. Due to different social norms and conditions, prevention strategies differ from country to country. In other countries, most hepatitis B infection takes place during adolescence, transmitted horizontally through direct contact such as sexual activity. If they had been inoculated against hepatitis B as babies, it would have been like giving birth control to an old woman: a superfluous action.

When infected by hepatitis, 90% of victims show no symptoms. Blood screening is the best way to identify chronic carriers so early treatment can be administered.
Down through the generations?
Further analysis showed that over half of those infected with hepatitis B in Taiwan acquired it in their early childhood. Among those people, half got it via "vertical transmission" from the mother at birth and the other half were directly infected by the age of two. Back then in Taiwan, 15% to 20% of expectant mothers were hepatitis B carriers. If this route of infection were not cut off, the disease would continue to be passed from generation to generation.
"If a person can recover from hepatitis B naturally and produce antibodies, the complications will not be severe, so the main focus of prevention is aimed at the chronic carrier. And the age of infection is a principal factor determining whether a person will become a chronic carrier," says Chen, pointing out that the earlier the age of hepatitis B infection, the fewer the symptoms, but also the greater the likelihood of becoming a carrier. The carrier will gradually show hepatitis symptoms in his twenties or thirties, which could become life-threatening cirrhosis or liver cancer in his forties or fifties. As many as 60% of carriers contract liver cancer, so of a total of 3 million carriers nationwide, perhaps 1.8 million will come down with it. The impact on society and the healthcare system is obvious.
But because the effects of a hepatitis B infection are not as readily visible as symptoms of, say, polio, people remain relatively impassionate, even doubtful, about the threats that loom in the next 20 or 30 years. Therefore health organizations must remind people time and again about the importance of hepatitis prevention and treatment.
Massive hepatitis B vaccinations were carried out under the banner of clinical trials. It might be considered the first such case in Taiwan's public health history. At that time laws and regulations regarding clinical trials were few and far between, so even the consent forms had to be translated by Chen himself. But though the vaccinations weren't mandatory, public acceptance of the program was considerable. And the vaccination rate has since then risen from 90% to 95% (98% in Taipei). Not counting premature births and people with congenital disease who are not suited for such vaccination, the number who actually refuse vaccination are few indeed.
"Cooperation among government and public health employees, doctors and the general public is very good, almost flawless," says Chen, giving Taiwan's hepatitis B prevention program a 100% thumbs up. But he doesn't mince words: if this program had been initiated today, it would not have been as effective due to considerations of human rights and medical risk.
Battling a public enemy
After 20 years of steadfast combat, Taiwan has achieved significant results in hepatitis B prevention.
It is estimated that the number of hepatitis B carriers in Taiwan has dropped from 3 million to 2.5 million in the last two decades, a drop of 500,000.
In addition, serum epidemiology studies conducted every five years by the pediatrics division at NTU show that the carrier rate for children under 18 in Taiwan has dropped sharply: as of 2004 it was under 0.6%, and the incidence of juvenile liver cancer has fallen by more than 75%. It is estimated that the number of chronic hepatitis B sufferers in this new generation will be reduced by 85% between 2004 and 2014.
"We expect that the hepatitis B carrier rate among those born after 1984 will be lower than 0.1%. Taiwan will gradually escape the grip of hepatitis B," says Chen.
Taiwan's experience has become a paradigm for global hepatitis B prevention. According to UN figures for 2002, 128 countries have followed Taiwan's lead, having initiated full-scale hepatitis B vaccinations.
Still a national disease
Although Taiwan has been successful in hepatitis B prevention, its fight against the "national disease" is not over. Now, liver disease still remains among the top ten causes of death among Taiwan's citizens.
Because HBV is so stubborn, once a person is infected, treatment options are limited. Numerous drugs have been developed, such as interferon a and various nucleoside analogs, but the former has many side effects and drug resistance easily develops with the latter. The efficacy of treatment is not great.
"The average age of onset for liver cancer patients in Taiwan is 54, but usually they were already infected with hepatitis B in their infancy. It has become an important issue among medical circles to identify the 60% of these carriers who are at high risk for liver cancer.
Celebrities like singer Simon Hsueh, International Community Radio Taipei DJ David Wang and chef Fu Pei-mei died of liver cancer at the peaks of their careers, while hepatitis B carriers like former Mainland Affairs Council chairman Su Chi and legislator Kao Chin Su-mei have gradually recovered after liver cancer surgery.
Why different fates for carriers of the same virus?
According to Chen, research has shown that the occurrence of liver cancer is higher among those with high virus counts (over 10,000 HBV per milliliter of blood).
Aside from virus count, the genetic makeup of the host is also an important factor. "The genetic interactions between virus and host differ from person to person. We know that liver cells that have been more seriously harmed by the virus are more likely to become cancerous. As to why some people's cells are more easily damaged and why some can be lifelong carriers without ever becoming sick, we still await the answers."
Targeting the number two killer
Of chronic hepatitis, cirrhosis and liver cancer cases in Taiwan, over 80% stem from hepatitis B while 15% are cased by hepatitis C. But there are also those who suffer from both diseases.
Following the great headway that has been made with hepatitis B, sights are now being increasingly set on the number-two killer, hepatitis C. At present there are about 400,000 to 500,000 hepatitis C carriers in Taiwan.
Vaccine development for hepatitis C is difficult because of the virus's propensity to mutate quickly, so we have to start by cutting off routes of infection. Fortunately, hepatitis C is not as infectious as hepatitis B: its principal vector is direct infection through needles and blood transfusions, so it's relatively easy to block.
Chen, in cooperation with the central government's Development Center for Biotechnology, came up with a locally developed hepatitis C screening reagent. Beginning in 1992, blood donation centers throughout Taiwan have been screening the blood of donors for hepatitis C. Estimating from the former 15-20% infection rate of blood transfusion recipients, each year some 5000 fewer people have contracted hepatitis C from transfusions.
In addition, the results of hepatitis C treatment are more effective. Of six genotypes, four can be treated with interferon in combination with the antiviral drug ribavirin, boasting a cure rate of 90%. In 1991, NTU Hospital was the first to develop this combined treatment, which has become a standard model for hepatitis C treatment worldwide.
Building a research base
Taiwan's first group of babies inoculated with the hepatitis B vaccine in 1984 are now 23 years old. No antibodies have been detected in their bodies, and therefore some people worry whether the vaccine's protective power continues to exist.
"We are closely monitoring the situation," says Chen. Not being able to detect antibodies does not necessarily mean that there is no resistance. The proof of the pudding is in the eating, and as of now the Department of Health's examinations have not found an increase in hepatitis prevalence.
Chen has shown great success in the battle against hepatitis B. Nevertheless, the war is not yet over, and he continues to fight against the crafty, mercurial virus and its enigmatic pathological mechanisms.
Why is it that the younger one is when infected with hepatitis B, the greater the chance for chronic infection? Why is it the opposite for hepatitis C? How does chronic infection lead to fibrosis and cirrhosis? Why does cirrhosis easily lead to liver cancer? Why does the post-treatment relapse rate for liver cancer remain so high? Unsolved riddles abound.
"In addition to the proteins, virus antigens and antibodies of the past, now we can add genetic makeup to the mix when looking at these problems," says Chen, aiming to gain further understanding of how to block the disease process. He is confident that he will see results in his lifetime.
Chen Ding-shinn, who has devoted the best years of his life to hepatitis B prevention, is like an old tree firmly rooted in its native soil. He will continu to reach new heights as he keeps on researching hepatitis, guiding and fostering new students, and defending the people of Taiwan.
Education School of Medicine NTU College of Medicine
Occupation Professor at NTU's Hepatitis Research Center
Academic honors
Outstanding Scientist Award, Executive Yuan (1984)
Nineteenth Class of Academicians, Academia Sinica (1992)
US National Academy of Sciences, Overseas Academician (2005)
Caring Physician of the World award, World Medical Association (2005)
Trieste Science Prize, Academy of Sciences for the Developing World (2006)






